By: Robyn Woidtke, MSN-Ed, RN, RPSGT, CCSH, FAAST
It’s hard to be a patient! A new approach using an adherence pyramid.
Each patient’s experience is different! Our lived lives, backgrounds, cultural influences, trust and distrust in the medical system, social determinants of health, age, and gender. This is the short list. It is virtually impossible to capture the enormity of the variety of patients who pass through the sleep center doors to obtain treatment for their condition. Whether it is sleep apnea, restless legs syndrome, narcolepsy, or insomnia, sometimes, the journey to get to the specialist is daunting. I recently came across an article that proposes an approach to helping patients adhere to medications. It struck me that this might be adopted in our field.
Lack of adherence to medically recommended treatment causes an increase in healthcare costs and impacts the quality of life. Non-adherence to medications for chronic conditions is upwards of 50-60%.1 According to a 2012 RAND2commentary, it is also interesting that many physicians don’t address non-adherence for multiple reasons, such as a lack of questioning the patient or feeling uncomfortable entering the patient’s “territory”.
Adherence is multifaceted and encompasses difficulties in understanding the condition, what needs to be done for self-management, self-efficacy, and a lack of resources, such as the inability to pay for medications and access to pharmacies.
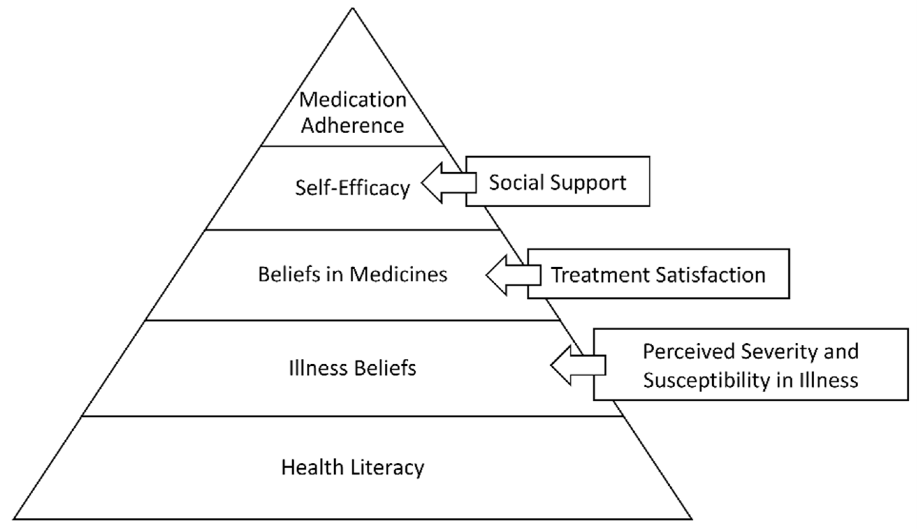
An article from 20223 proposed a new hierarchical approach to medication adherence (Figure 1). This model may be applicable to individuals receiving therapy for sleep apnea. At the base, everyone should have a basic understanding, i.e., health literacy for the condition they are diagnosed with. From there, the pyramid continues until adherence is achieved. This model thus needs to build on each section to reach the top. Let’s take a look at how sleep apnea might be impacted, let’s start at the bottom.
Figure 1 from Unni E, Bae S. Exploring a New Theoretical Model to Explain the Behavior of Medication Adherence. Pharmacy. 2022; 10(2):43. https://doi.org/10.3390/pharmacy10020043 (Open Commons)
Health Literacy: Health literacy and knowledge about sleep apnea are known factors in non-adherence. Thus, the proposed model would need to include either an assessment of health literacy regarding sleep and sleep apnea or provide adequate education, followed by an assessment. Several recent questionnaires have been proposed and evaluated; these include the Sleep Health Literacy Scale4 the Survey of OSA Functional Health Literacy (SOFHL).5
The next item in the pyramid is “illness beliefs”. For some patients, believing in their diagnosis or having faith in the medical system is important to initiating and continuing treatment. The COVID-19 pandemic only accelerated this distrust, not only among physicians, but also in science in general. A project at the PEW institute looking at the trust issue. The Forward Movement Project aims to explore the issue of distrust and foster conversations about repair.6-7
Beliefs in medicine (Sleep apnea treatment), this is a bit different than trust or illness beliefs, once a patient believes that they have a condition and trust their physician to treat them, they need to believe that the treatment works and also, works for them. Patient are also concerned about side effects. I know many of us in the sleep field have heard this from patients, i.e. I don’t feel any better. Demonstrating the value of treatment to patients is important. Maybe helping them to understand that it’s not just treating the obstructive sleep apnea (OSA), but that treatment may prevent a whole host of health related adverse consequences. A very recent article on OSA patients coming into the ER found that patients with OSA typically faired worse than those without. However, limitations in this study included not knowing the severity of OSA or treatments.8
Self-Efficacy: Quite a bit of work regarding self-efficacy in the OSA population exists, but too lengthy for this article to review. In the above model, self-efficacy also encompasses social support.9 A recent study by Khan et al.10 examined the role of support in adherence to continuous positive airway pressure (CPAP). The authors found that caregivers with appropriate training can aid in adherence to CPAP therapy.
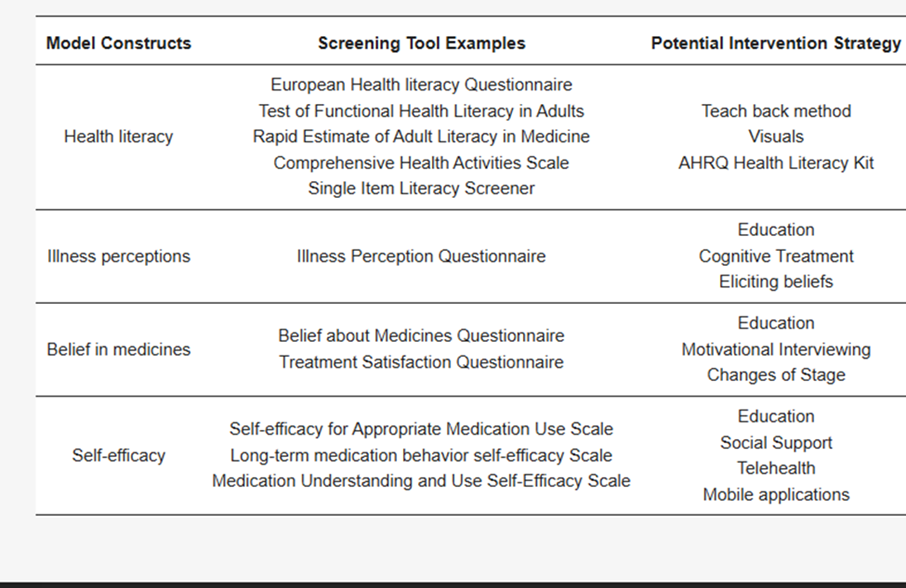
The potential use of this model to enhance long-term adherence to sleep apnea therapy may lead to improved patient outcomes. The referenced article also provides some helpful hints and examples to aid clinicians in adopting this framework (Figure 2). However, the sleep literature may provide alternative tools for screening and specific interventional strategies.
Figure 2 from Unni E, Bae S. Exploring a New Theoretical Model to Explain the Behavior of Medication Adherence. Pharmacy. 2022; 10(2):43. https://doi.org/10.3390/pharmacy10020043 (Open Commons)
In conclusion, adherence to treatment is difficult. Patients need ongoing support and assessment, however, it’s important to start at the baseline to formulate the foundation for successful adoption, activation and engagement for treatment.
References
- Unni E, Bae S. Exploring a New Theoretical Model to Explain the Behavior of Medication Adherence. Pharmacy. 2022; 10(2):43. https://doi.org/10.3390/pharmacy10020043
- Bell DS, Adamson DM. When Patients Don’t Take Their Medicine: What Role Do Doctors Play in Promoting Prescription Adherence? Rand.org. Published August 29, 2012. Accessed June 18, 2025. https://www.rand.org/pubs/commentary/2012/08/when-patients-dont-take-their-medicine-what-role-do.html
- Ellender CM, Le Feuvre S, Boyde M, Duce B, Winter S, Hukins CA. Adequate health literacy is associated with adherence to continuous positive airway pressure in adults with obstructive sleep apnea. Sleep Adv. 2021;2(1):zpab013. Published 2021 Sep 1. doi:10.1093/sleepadvances/zpab013
- Feldman EL, Slavish DC. Initial development of a sleep health literacy scale. Sleep Health. 2024;10(6):683-690. doi:https://doi.org/10.1016/j.sleh.2024.08.001
- Robbins R, Hays RD, José Luís Calderón, et al. The Development and Psychometric Evaluation of the Survey of Obstructive Sleep Apnea Functional Health Literacy. Sleep Medicine Research. 2021;12(1):64-73. doi:https://doi.org/10.17241/smr.2021.00885
- Rebuilding trust in medical science: How doctors and scientists can bridge the misinformation divide. AAMC. Published 2025. https://www.aamc.org/news/rebuilding-trust-medical-science-how-doctors-and-scientists-can-bridge-misinformation-divide
- Hooper MW. From Distrust to Confidence: Can Science and Health Care Gain What’s Missing? Pew.org. Published October 17, 2024. Accessed June 18, 2025. https://www.pew.org/en/trend/archive/fall-2024/from-distrust-to-confidence-can-science-and-health-care-gain-whats-missing
- Sun M, Zhang X, Liu YC, Pei J, Fan H, Guo J. Clinical characteristics and resource utilization of emergency department patients with obstructive sleep apnea. Guo Y, ed. PLOS One. 2025;20(6):e0326194. doi:https://doi.org/10.1371/journal.pone.0326194
- Ghose SM, Dzierzewski JM, Dautovich ND. Sleep and self-efficacy: The role of domain specificity in predicting sleep health. Sleep Health. Published online November 2022. doi:https://doi.org/10.1016/j.sleh.2022.09.008
- Khan ND, Todem D, Eduard Poltavskiy, Shireesha Bottu, M. Safwan Badr, Adesuwa Olomu. Impact of patient and family engagement in improving continuous positive airway pressure adherence in patients with obstructive sleep apnea: a randomized controlled trial. 2022;18(1):181-191. doi:https://doi.org/10.5664/jcsm.9534